
Description
Hepatitis disease commonly known as jaundice. Actually hepatitis is liver inflammation (liver) caused by various factors. Factors that cause hepatitis or jaundice, among others, is a viral infection, metabolic disorders, alcohol consumption, autoimmune diseases, results complications from other diseases, side effects from the consumption of drugs and the presence of parasites in the liver,
Symptoms
One of the symptoms of hepatitis is the emergence of yellow color on the skin, nails and the whites of the eyeball.
Therapy
Usual medical therapy medical therapy is usually given to patients with hepatitis among other diseases, bed rest, healthy diet, and administration of drugs and antiviral.
Visit this links
Monday, November 23, 2009
Hepatitis - jaundice
Friday, November 20, 2009
Anthrax
 Description
Description
Anthrax is a bacterial disease caused by Bacillus anthracis, which lives in soil. Such as bacterial spores to survive the fierce conditions. Spores thrive in a colony in the animal or human body.
Anthrax sometimes attack livestock away from the man, but - as known in the 2001 anthrax attack the United States - fear anthrax as a weapon of modern biology. Atraks transmission through meat or skin anthrax-affected animals eaten by humans.
Symptoms
The average incubation period of anthrax is more than 7 days, 60 days can be even more depending on the duration of symptoms is formed. Patients usually have symptoms of anthrax, among others, swollen, fever, anxiety, headaches, and generally feel uneasy.
Medical
If diagnosed early, anthrax easily treated with atibiotik. But sometimes, people ignore the early symptoms of anthrax before they actually had symptoms become more severe. Antibiotics for anthrax can kill bacteria, but antibiotics have no effect on anthrax toxin.
Thursday, November 19, 2009
Acne
 Description
Description
Acne is caused by dead skin cells or because the production of excessive oil glands. There are 3 types of acne:
1. Blackheads
Caused blackheads pores clogged because the dead skin cells and the production of excessive oil glands. Other causes of sweating, hot and humid air.
2. Common acne
Small bulge, pink. Caused by clogged pores bacteria. Another cause for dirty air or stress.
3. Acne stone
Tonjonlannya hard and big. Cause kalenjar oil production in excess skin or sensitive skin.
Symptoms
As known acne appears on the face and shoulders, but can spread to the trunk, arms and legs.
Medical
X-ray therapy is not recommended to overcome acne. This therapy can damage the skin. If the acne blackheads appearing type compressed enough warm water. The goal soften blackheads making them easier to lift. If acne in or stones should take antibiotics at the direction of a dermatologist.
Wednesday, March 19, 2008
Doctors Should Ask About Cocaine Use When Younger Patients Present With Chest Pains
In a bid to improve management of patients who present with chest pain and other heart attack symptoms, the American Heart Association (AHA) has issued a scientific statement recommending doctors ask about cocaine use when they examine younger patients with chest pains and who have no obvious risk factors for heart disease.
The statement is published as a paper in an early online issue of Circulation, the journal of the AHA, and is authored by Dr James McCord, chair of the statement writing committee and cardiology director of the chest pain unit for the Henry Ford Medical System in Detroit, Michigan, and colleagues.
McCord explained that if doctors suspect a heart attack, then they should rule out cocaine use early on because cocaine exposure changes what is safe and what is not. The statement emphasizes in particular that:
- Clot-busters and beta-blockers are dangerous for patients who have been exposed to cocaine.
- Bare metal stents rather than drug-eluting stents should be used in long-term cocaine users.
- Most cocaine-associated chest pain is not a heart attack.
- Patients who have been exposed to cocaine should be placed under observation for 9 to 12 hours.
Research shows that chest pain that is associated with cocaine use tends to appear within three hours of taking the drug, but the chemical residue stays in the body for a minimum of 18 hours and can continue to present problems, said McCord. Also, doctors have more difficulty diagnosing heart attacks using electrocardiographs of younger patients, he explained.
Cocaine-associated emergency department visits went up by 47 per cent between 1999 and 2002, said the authors, which means that the number of cocaine users that doctors are likely to come across as a result of such admissions will probably increase.
A common method for diagnosing and treating heart attacks is to take the patient into the catheterization lab (the "cath lab"), which has the equipment that allows the doctor to insert a thin tube or catheter into a heart artery and then use imaging techniques to see where the blockage might be, and then inflate a small balloon to open the the artery.
Where a cath lab is not available, a doctor may give a patient who appears to have had a heart attack a clot busting drug instead. However, if the patient is a recent cocaine user there is an added risk of bleeding into the brain because of the higher blood pressure induced by the cocaine. So this procedure should only be used if the doctor is absolutely certain the patient has indeed had a heart attack, said the authors.
Beta-blockers are used to reduce blood pressure without causing narrowing of the arteries. But in patients who have recently been using cocaine and who present with chest pain, beta-blockers may actually produce the opposite effect: they could increase blood pressure and make the arteries already narrowed by cocaine even narrower. This has been shown to have potential fatal consequences in studies using animals, said McCord.
Drug eluting or bare metal stents are used to restore blood flow to the heart where there is no arterial blockage. Studies have shown that long term cocaine users fitted with stents have a tendency to lapses in taking the regular medication needed to stop drug-eluting stents becoming blocked, and that is why the statement recommends such patients be fitted with bare metal ones only.
Cocaine can worsen the effects of a heart attack, said the authors, because it increases the heart's need for oxygen, elevating heart rate, blood pressure and contraction power at each beat. But at the same time the drug also constricts blood vessels and makes it harder for the heart to get the oxygen it needs. This increases risk of clotting and manifests as angina, which is felt as chest pain.
The statement draws attention to other conditions that can develop alongside chest pain and heart attacks with cocaine users, and it is important that these are also looked for as they can be crucial to the treatment that is followed. For instance, one condition that can accompany cocaine use is aortic dissection (a tear in a blood vessel that can be fatal), another is bleeding into the lung ("crack lung").
Other symptoms that patients who use cocaine also report having alongside chest pains are shortness of breath, palpitations, feelings of anxiety, nausea, dizziness and sweating profusely. These are very similar to heart attack.
Monday, February 25, 2008
The Changing Face of AIDS
The rapidly mutating virus developed resistance to the drugs that were used to suppress it. In the mid 1990’s drug “cocktails,” multi drug combinations of antiretroviral drugs were able to provide barriers to mutation. The number of deaths for AIDS patients dropped dramatically and long term aspects of the disease changed. Victims could expect longer life spans though they would require medication the rest of their lives.
The longer life expectancy of AIDS patients presented another set of problems. AIDS patients are living longer, but they are aging faster. Those in the 50 to 60 age group who suffer from AIDS, have the health issues that most people do not experience until they are a decade older.
The number of AIDS sufferers over the age of 50 has increased by 77% from 2001 to 2005, and now more than a quarter of the approximately one million active AIDS cases in this country are advanced in age. Of 5,049 patients who began AIDS therapy between 1995 and 2004, 997 were over the age of 50, 1,834 were 40-49 and the rest were between 18-39 years of age. AIDS presented new challenges to the medical community in the 70’s and 80’s and now the problems presented in the aging AIDS population is again challenging the medical community.
There is presently no data that specifically compares the onset of geriatric diseases between AIDS and non AIDS patients, but the medical community says that people in their mid-50’s, without AIDS, usually do not have heart disease or diabetes associated with lipodystrophy or oesteoporosis without additional risk factors.
Lipodystrophy is a side effect of the drugs that keeps HIV in check. It rearranges fat in the body and can lead to the sunken eyes and cheeks usually associated with advanced age. It can lead to insulin resistance and raise triglyceride levels. Individuals on AIDS therapy treatment are usually treated with corticosteroids to protect against other opportunistic infections that prey on HIV weakened immune systems. This can lead to a bone disease, vascular necrosis, and the necessity for hip replacement surgery. Other aging problems with HIV are the development of memory deficits and liver and kidney disease.
In a Jan 6, 2008 article in the International Herald Tribune, Jane Gross quotes Dr. Tom Barrett, medical director of Howard Brown, “All we can do right now is to make inferences from thing to thing to thing. They might have gotten some of these diseases anyway. But the rates and the timing, and the association with certain drugs, makes everyone feel that this is a different problem.”
Why is this happening? There haven’t been any studies to provide sound statistics of what problems are related to AIDS. Only recently have there been enough aging AIDS patients to study. The initial assumptions are that those who have survived with the AIDS infection, have immune systems and organs that first took a beating from the disease, and then were further damaged by the toxicity of the antiretroviral drugs which they took to survive the disease.
With lack of research, patient care suffers. Barrett says the incidence of osteoporosis warrants routine screening. However, in the United States, Medicare, Medicaid and most private insurers will not cover bone density tests for middle aged men.
The New York-based AIDS Community Research Initiative of America, in trying to provide help and assistance to older individuals with AIDS, found that depression, which is common to the elderly, is even higher among longtime AIDS survivors. They often grow despondent because of health issues and the deaths of friends and associates.
Mary Engel, writing in the Los Angeles Times on February 5, 2008 quotes Los Angeles resident and long time survivor Thomas Woolsey, 59, “Everybody I knew died in the late ‘80’s or early ‘90’s. It sounds like I’m the lucky one, but I don’t really think so. What good is a life without any friends?”
Thursday, November 22, 2007
ASTHMA
Asthma is defined as a respiratory disease caused by narrowing of the air passages. It is synonymous with difficulty in breathing, tightness of chest, nasal irritation, coughing and wheezing. The first person to use it in reference to a medical condition was Hippocrates in 450 BC, and he believed that tailors, anglers and metalworkers were more likely to be affected by the disease. Although much research has been done since, the inflammatory component of asthma was recognized only in the 1960s.
Today, asthma affects as much as 15% of the Canadian population (and this is true of other developed countries too) and has increased four fold in the last 20 years. Various reasons can be identified for this increase - Of course better diagnosis and facilities along with a greater awareness regarding the disease have played a major role. But, one cannot deny the part of increased environmental pollution. Researchers have been working on the relation between the environment and human health since long and the air we breathe is the primary cause for lung diseases like asthma, rhinitis, COPDs, etc. that affect us today.
Approximately 10 to 15% of the adults affected by the disease report an aggravation of their symptoms while at work and an improvement when away, which implies that they may be suffering from Occupational Asthma. Thus, when an individual’s Asthma is caused, not aggravated, by workplace materials, it is defined as Occupational Asthma. In the USA, OA is considered the most common occupational lung disease. At present, over 400 workplace substances have been identified as having asthmagenic or allergenic properties. Their existence and magnitude vary from region to region and the type of industry and can be as varied as wood dust (cedar, ebony, etc.), persulfates (Hairsprays), zinc or even seafood like prawns. For example, in France the industries most affected in order of importance are Bakeries and cake-shops, automobile industry and hairdressers, whereas in Canada the principal cause is wood dust, followed by isocyanates.
SIGNS & SYMPTOMS
Less than five years of exposure to an occupational agent can be enough for the appearance of the first OA symptoms. This depends on whether the reason for the OA to occur was exposure to the causative agent over a period of time (with a latency period) or a single exposure to an irritant but at a very high concentration (without latency period). Both eventually result in OA. Coughing, wheezing, nasal irritation, difficulty in breathing, tightness of chest are the most common symptoms and can be recognized more easily by asking oneself the following questions:
- Are any of the above symptoms recurrent/chronic?
- Are they present at work?
- Do they worsen towards the end of the work day and/or end of the week?
- Does the employee/worker feel an improvement in his condition when away from work, on vacation or on weekends?
If these symptoms persist, the person is most likely suffering from OA. However, one must be aware that this could also be because the person is already suffering from asthma and his condition was simply aggravated by workplace irritants (Work-aggravated asthma). In this case, although he will suffer similar consequences as someone who is suffering from OA (loss of work, medical expenses, etc.), his disease cannot be considered as having an occupational origin.
PREVENTION & TREATMENT
According to the Canadian Centre for Occupational Health and Safety (CCOHS) better education of workers, management, unions and medical professionals is the key to the prevention of OA. This will enable them to identify the risk factors and put in place preventive measures like masks or exposure limits, etc.
Recovery is directly dependent on the duration and level of exposure to the causative agent. Depending on the severity of the case, the condition of the patient can improve dramatically during the first year after removal from exposure.
Three basic types of procedures are used for treating the affected workers:
1) Reducing exposure
This method is most effective for those affected by irritant-induced OA. Thus, by reducing their exposure duration and level to the causative agent, the probability of suffering another reaction is lowered. But exposure can be reduced in other ways like making use of face masks or providing better ventilation. Now, more and more di-isocyanate free spray paints are available. Similarly, most hospitals and healthcare companies have exchanged latex gloves for other materials. Thus, reducing exposure to known asthmagens can also be used as a preventive measure.
2) Removal from exposure
Persons affected by OA that occurred after a latency period, whether a few months or years, must be immediately removed from exposure to the causative agent. This is their only chance of recovery. However, this entails severe socio-economic consequences for the worker as well as the employer due to loss of job, unemployment, compensation issues, quasi-permanent medical expenditures, hiring and re-training of new personnel, etc. Also, according to recent research the probability that those who suffer from OA remain unemployed longer than those who suffer from non-occupational asthma is higher. One solution to this problem is relocating the employee in the same company away from the causative agents.
3) Medical and pharmacological treatment
Anyone diagnosed with Asthma will have to undergo medical treatment. This is complementary to either removing or reducing the patient’s exposure to the causal agents. Two types of medication can be used:
- Relievers or bronchodilators
-
Short-acting beta-agonists like salbutamol or terbutaline or long-acting beta-agonists like salmeterol and formoterol or anticholinergic, etc. dilate airways which relieve the symptoms thus reducing the severity of the reaction. Some patients also use it just before work to avoid a drop in the FEV1.
- Preventers
Anti-inflammatory agents like corticosteroids, LKTRA or mast cell stabilizers can be used depending on the severity of the case.
Gigantism
Gigantism or giantism, (from Greek gigas, gigantas "giant") is a condition characterized by excessive height growth and bigness significantly above average height. As a medical term, gigantism is rarely used except to refer to the rare condition of pituitary gigantism due to prepubertal growth hormone excess. There is no precise definition of the degree of height that qualifies a person to be termed a "giant." The term has been typically applied to those whose height is not just in the upper 1% of the population but several standard deviations above mean for persons of the same sex, age, and ethnic ancestry. Typical adult heights of Americans of European descent to whom the term might be applied are 2.25 - 2.40 metres (7'6" - 8 feet). The term is not applied to those whose heights appear to be the healthy result of normal genetics and nutrition.
Pituitary growth hormone excess is the single condition that accounts for nearly all cases of pathologic extreme height. The excess growth hormone usually results from oversecretion by a group of somatotrope cells of the anterior pituitary gland (termed a "somatotrope adenoma"). These cells do not respond to normal controls of growth or function. They grow very slowly, so that for many years the only effects of such an adenoma are the secretion of excessive growth hormone. Over decades, such an adenoma may reach a large enough size (20 mm or more in diameter) to cause headaches, impair vision, or damage other pituitary functions. Many years of growth hormone excess can cause other problems as well.
The primary effect of growth hormone excess in childhood is excessive growth, but the extreme height is accompanied by a characteristic physique recognizable to an endocrinologist. The typical physique involves heavy, thick bones, with large hands and feet and a heavy jaw. Once puberty is complete and adult height is achieved, continued thickening of the skin and growth of the jaw results in a combination of features referred to as acromegaly.
If a physician suspects pituitary gigantism or acromegaly, the simplest diagnostic screening test is measurement of insulin-like growth factor 1 in the blood. This is usually quite elevated but levels must be interpreted in relation to age and pubertal status. Additional confirmatory testing may include magnetic resonance imaging (MRI) of the pituitary to look for a visible adenoma, and suppressibility of growth hormone levels by glucose. Treatment depends on the size of the adenoma and may involve removal by a neurosurgeon, drugs such as octreotide or bromocriptine, or radiation. Treatment is discussed in more detail in the acromegaly article.
Childhood pituitary gigantism is a rare condition, and those affected are often unusual enough to attain a degree of celebrity status (for example, André the Giant and The Great Khali). Acromegaly is the term used for the condition of growth hormone excess when it occurs in adults. Acromegaly is a far more common disease in adults than pituitary gigantism is in children.
Children who are excessively tall are often referred to as Giantigionists. The majority of children who seem excessively tall or large to their parents usually have a combination of simple familial tallness and childhood obesity.
Early onset of obesity results in above-average growth in mid-childhood, such that over half of overweight children have heights in the 70 - 99 percentile range at around 10 years of age. The adult heights achieved by these children are what would be expected from their families because the excess mid-childhood growth is offset by attenuation of the pubertal growth spurt.
Precocious puberty and a variety of conditions associated with excessive amounts of testosterone or estrogen in childhood will result in tallness by mid-childhood. However, the acceleration of bone maturation by the early rise of estradiol results in early completion of growth, and adult heights for these children may actually be below average for genetic potential.
Extra sex chromosomes (beyond the normal two) with therefore extra copies of the SHOX gene (beyond the normal two) usually results in enhancement of height growth. The most common of these karyotypes are 47,XXY (Klinefelter syndrome), 47,XYY, and 47,XXX. The added height increment is usually modest.
Hypogonadism is the condition of deficiency of sex hormones due to reduced function of the testes or ovaries at adolescence. When secretion of testosterone or estradiol remains below average throughout the teenage years, a taller adult height will be gradually achieved by extra growth of the arms and legs. This long-limbed tallness is termed "eunuchoid" tallness, but rarely adds more than 25 mm - 75 mm (1-3 in) to adult height. The extra growth is prevented if the child is given appropriate replacement of testosterone or estrogen from early adolescence.
A very rare but more extreme version of "eunuochoid" tallness occurs when a mutation of the estrogen receptor reduces the response of the bones to estradiol. Estradiol is a byproduct of testosterone in both males and females, and is the most potent accelerator of bone maturation and closure known. If a person fails to respond to estrogen, growth can continue until late-20s or longer, and the affected person can reach 8 feet or more in height. Estrogen resistance is the only other endocrine condition that can rival growth hormone excess in producing gigantism. In contrast, the tallness associated with the more common androgen insensitivity syndrome averages only a few inches, as estradiol is not produced directly but rather through conversion from androgens by aromatase.
Marfan syndrome is an uncommon genetic disease due to an inherited defect of connective tissue. In addition to moderate tallness, persons with this condition usually have a slender body build with unusually long fingers (arachnodactyly). Many can also develop a dislocaton of the lens of the eye or, more seriously, a progressive deterioration of the walls of the aorta which can result in sudden death in adulthood. It is usually inherited as an autosomal dominant trait.
Sotos syndrome resembles acromegaly in its mild distortion of facial growth. In addition to tallness, the chief characteristics are large head size, slow development, and autosomal-dominant inheritance.
There are about 50 even rarer genetic syndromes in which childhood growth is above average. These conditions are often associated with developmental delay or other more serious problems, and adult height may or may not be mildly increased.
Genetic Disease
A genetic disorder is a condition caused by abnormalities in genes or chromosomes. While some diseases, such as cancer, are due to genetic abnormalities acquired in a few cells during life, the term "genetic disease" most commonly refers to diseases present in all cells of the body and present since conception. Some genetic disorders are caused by chromosomal abnormalities due to errors in meiosis, the process which produces reproductive cells such as sperm and eggs. Examples include Down syndrome (extra chromosome 21), Turner Syndrome (45X0) and Klinefelter's syndrome (a male with 2 X chromosomes). Other genetic changes may occur during the production of germ cells by the parent. One example is the triplet expansion repeat mutations which can cause fragile X syndrome or Huntington's disease. Defective genes may also be inherited intact from the parents. In this case, the genetic disorder is known as a hereditary disease. This can often happen unexpectedly when two healthy carriers of a defective recessive gene reproduce, but can also happen when the defective gene is dominant.
Currently around 4,000 genetic disorders are known, with more being discovered. Most disorders are quite rare and affect one person in every several thousands or millions. Cystic fibrosis is one of the most common genetic disorders; around 5% of the population of the United States carry at least one copy of the defective gene. Some types of recessive gene disorder confer an advantage in the heterozygous state in certain environments.
Genetic diseases are typically diagnosed and treated by geneticists. Genetic counselors assist the physicians and directly counsel patients. The study of genetic diseases is a scientific discipline whose theoretical underpinning is based on population genetics.
Where genetic disorders are the result of a single mutated gene they can be passed on to subsequent generations in the ways outlined in the table below. Genomic imprinting and uniparental disomy, however, may affect inheritance patterns. The divisions between recessive and dominant are not "hard and fast" although the divisions between autosomal and X-linked are (related to the position of the gene). For example, achondroplasia is typically considered a dominant disorder, but children with two genes for achondroplasia have a severe skeletal disorder that achondroplasics could be viewed as carriers of. Sickle-cell anemia is also considered a recessive condition, but carriers that have it by half along with the normal gene have increased immunity to malaria in early childhood, which could be described as a related dominant condition.
Genetic disorders may also be complex, multifactorial or polygenic, this means that they are likely associated with the effects of multiple genes in combination with lifestyle and environmental factors. Multifactoral disorders include heart disease and diabetes. Although complex disorders often cluster in families, they do not have a clear-cut pattern of inheritance. This makes it difficult to determine a person’s risk of inheriting or passing on these disorders. Complex disorders are also difficult to study and treat because the specific factors that cause most of these disorders have not yet been identified.
On a pedigree, polygenic diseases do tend to “run in families”, but the inheritance does not fit simple patterns as with Mendelian diseases. But this does not mean that the genes cannot eventually be located and studied. There is also a strong environmental component to many of them (e.g., blood pressure).
Saturday, November 17, 2007
Breast cancer is a cancer of the glandular breast tissue.

Worldwide, breast cancer is the fifth most common cause of cancer death (after lung cancer, stomach cancer, liver cancer, and colon cancer). In 2005, breast cancer caused 502,000 deaths (7% of cancer deaths; almost 1% of all deaths) worldwide. Among women worldwide, breast cancer is the most common cause of cancer death.
In the United States, breast cancer is the third most common cause of cancer death (after lung cancer and colon cancer). In 2007, breast cancer is expected to cause 40,910 deaths (7% of cancer deaths; almost 2% of all deaths) in the U.S. Among women in the U.S., breast cancer is the most common cancer and the second-most common cause of cancer death (after lung cancer). Women in the U.S. have a 1 in 8 lifetime chance of developing invasive breast cancer and a 1 in 33 chance of breast cancer causing their death. In the U.S., both incidence and death rates for breast cancer have been declining in the last few years. Nevertheless, a U.S. study conducted in 2005 by the Society for Women's Health Research indicated that breast cancer remains the most feared disease, even though heart disease is a much more common cause of death among women.
The number of cases worldwide has significantly increased since the 1970s, a phenomenon partly blamed on modern lifestyles in the Western world. Because the breast is composed of identical tissues in males and females, breast cancer also occurs in males, though it is less common.
Prevention

A. Phytoestrogens and soy
Phytoestrogens such as found in soybeans have been extensively studied in animal and human in-vitro and epidemiological studies. The literature support the following conclusions:
1. Plant estrogen intake, such as from soy products, in early adolescence may protect against breast cancer later in life.
2. Plant estrogen intake later in life is not likely to influence breast cancer incidence either positively or negatively.
B. Folic Acid C. Avoiding exposure to secondhand tobacco smoke
Treatment
The mainstay of breast cancer treatment is surgery when the tumor is localized, with possible adjuvant hormonal therapy (with tamoxifen or an aromatase inhibitor), chemotherapy, and/or radiotherapy. At present, the treatment recommendations after surgery (adjuvant therapy) follow a pattern. This pattern is subject to change, as every two years, a worldwide conference takes place in St. Gallen, Switzerland, to discuss the actual results of worldwide multi-center studies. Depending on clinical criteria (age, type of cancer, size, metastasis) patients are roughly divided to high risk and low risk cases, with each risk category following different rules for therapy. Treatment possibilities include radiation therapy, chemotherapy, hormone therapy, and immune therapy.
In planning treatment, doctors can also use PCR tests like Oncotype DX or microarray tests like MammaPrint that predict breast cancer recurrence risk based on gene expression. In February 2007, the MammaPrint test became the first breast cancer predictor to win formal approval from the Food and Drug Administration. This is a new gene test to help predict whether women with early-stage breast cancer will relapse in 5 or 10 years, this could help influence how aggressively the initial tumor is treated.
Stroke
Stroke (or cerebrovascular accident (CVA)) is the clinical designation for a rapidly developing loss of brain function due to an interruption in the blood supply to all or part of the brain. This phenomenon can be caused by thrombosis, embolism, or hemorrhage. In medicine, the process of being struck down by a stroke, fit, or faint is sometimes called an ictus [cerebri], from the Latin icere ("to strike"), especially prior to a definitive diagnosis.
Stroke is a medical emergency and can cause permanent neurological damage and death if not promptly diagnosed and treated. It is the third leading cause of death and the leading cause of adult disability in the United States and Europe. It is predicted that stroke will soon become the leading cause of death worldwide.
The symptoms of stroke can be quite heterogeneous, and patients with the same cause of stroke can have widely differing handicaps. Conversely, patients with the same clinical handicap can in fact have different underlying causes.
The cause of stroke causeing neurons to die or be seriously damaged, further impairing brain function.
Risk factors for stroke include advanced age, hypertension (high blood pressure), previous stroke or TIA (transient ischaemic attack), diabetes mellitus, high cholesterol, cigarette smoking, atrial fibrillation, migraine with aura, and thrombophilia. In clinical practice, blood pressure is the most important modifiable risk factor of stroke; however many other risk factors, such as cigarette smoking cessation and treatment of atrial fibrillation with anticoagulant drugs, are important.
Signs & Symptoms
The symptoms of stroke depend on the type of stroke and the area of the brain affected. Ischemic strokes usually only affect regional areas of the brain perfused by the blocked artery. Hemorrhagic strokes can affect local areas, but often can also cause more global symptoms due to bleeding and increased intracranial pressure.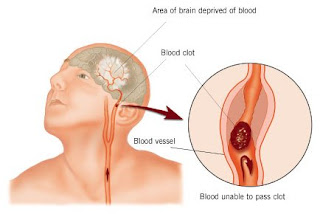
If the area of the brain affected contains one of the three prominent Central nervous system pathways—the spinothalamic tract, corticospinal tract, and dorsal column (medial lemniscus), symptoms may include:
- hemiplegia and muscle weakness of the face
- numbness
- reduction in sensory or vibratory sensation
In most cases, the symptoms affect only one side of the body. The defect in the brain is usually on the opposite side of the body (depending on which part of the brain is affected). However, the presence of any one of these symptoms does not necessarily suggest a stroke, since these pathways also travel in the spinal cord and any lesion there can also produce these symptoms.
In addition to the above CNS pathways, the brainstem also consists of the 12 cranial nerves. A stroke affecting the brainstem therefore can produce symptoms relating to deficits in these cranial nerves:
- altered smell, taste, hearing, or vision (total or partial)
- drooping of eyelid (ptosis) and weakness of ocular muscles
- decreased reflexes: gag, swallow, pupil reactivity to light
- decreased sensation and muscle weakness of the face
- balance problems and nystagmus
- altered breathing and heart rate
- weakness in sternocleidomastoid muscle with inability to turn head to one side
- weakness in tongue (inability to protrude and/or move from side to side)
If the cerebral cortex is involved, the CNS pathways can again be affected, but also can produce the following symptoms:
- aphasia (inability to speak or understand language from involvement of Broca's or Wernicke's area)
- apraxia (altered voluntary movements)
- visual field defect
- memory deficits (involvement of temporal lobe)
- hemineglect (involvement of parietal lobe)
- disorganized thinking, confusion, hypersexual gestures (with involvement of frontal lobe)
If the cerebellum is involved, the patient may have the following:
- trouble walking
- altered movement coordination
- vertigo and or disequilibrium
Loss of consciousness, headache, and vomiting usually occurs more often in hemorrhagic stroke than in thrombosis because of the increased intracranial pressure from the leaking blood compressing on the brain.
If symptoms are maximal at onset, the cause is more likely to be a subarachnoid hemorrhage or an embolic stroke.
Risk factors and prevention
Prevention of stroke can work at various levels including:
- primary prevention - the reduction of risk factors across the board, by public health measures such as reducing smoking and the other behaviours that increase risk;
- secondary prevention - actions taken to reduce the risk in those who already have disease or risk factors that may have been identified through screening; and
- tertiary prevention - actions taken to reduce the risk of complications (including further strokes) in people who have already had a stroke.
The most important modifiable risk factors for stroke are hypertension, heart disease, diabetes, and cigarette smoking. Other risks include heavy alcohol consumption (see Alcohol consumption and health), high blood cholesterol levels, illicit drug use, and genetic or congenital conditions. Family members may have a genetic tendency for stroke or share a lifestyle that contributes to stroke. Higher levels of Von Willebrand factor are more common amongst people who have had ischemic stroke for the first time. The results of this study found that the only significant genetic factor was the person's blood type. Having had a stroke in the past greatly increases one's risk of future strokes.
One of the most significant stroke risk factors is advanced age. 95% of strokes occur in people age 45 and older, and two-thirds of strokes occur in those over the age of 65. A person's risk of dying if he or she does have a stroke also increases with age. However, stroke can occur at any age, including in fetuses.
Sickle cell anemia, which can cause blood cells to clump up and block blood vessels, also increases stroke risk. Stroke is the second leading killer of people under 20 who suffer from sickle-cell anemia.
Men are 1.25 times more likely to suffer strokes than women, yet 60% of deaths from stroke occur in women. Since women live longer, they are older on average when they have their strokes and thus more often killed (NIMH 2002). Some risk factors for stroke apply only to women. Primary among these are pregnancy, childbirth, menopause and the treatment thereof (HRT). Stroke seems to run in some families.
Prevention is an important public health concern. Identification of patients with treatable risk factors for stroke is paramount. Treatment of risk factors in patients who have already had strokes (secondary prevention) is also very important as they are at high risk of subsequent events compared with those who have never had a stroke. Medication or drug therapy is the most common method of stroke prevention. Aspirin (usually at a low dose of 75 mg) is recommended for the primary and secondary prevention of stroke. Also see Antiplatelet drug treatment. Treating hypertension, diabetes mellitus, smoking cessation, control of hypercholesterolemia, physical exercise, and avoidance of illicit drugs and excessive alcohol consumption are all recommended ways of reducing the risk of stroke.
In patients who have strokes due to abnormalities of the heart, such as atrial fibrillation, anticoagulation with medications such as warfarin is often necessary for stroke prevention.
Procedures such as carotid endarterectomy or carotid angioplasty can be used to remove significant atherosclerotic narrowing (stenosis) of the carotid artery, which supplies blood to the brain. These procedures have been shown to prevent stroke in certain patients, especially where carotid stenosis leads to ischemic events such as transient ischemic attack. (The value and role of carotid artery ultrasound scanning in screening has yet to be established.)
info : wikipedia
Thursday, November 15, 2007
Heart Disease
Heart disease is an umbrella term for a number of different diseases which affect the heart and as of 2007 it is the leading cause of death in the United States, and England and Wales.

Type Of Heart Disease:
Cardiomyopathy
- Cardiomyopathy literally means "heart muscle disease" (Myo= muscle, pathy= disease) It is the deterioration of the function of the myocardium (i.e., the actual heart muscle) for any reason. People with cardiomyopathy are often at risk of arrhythmia and/or sudden cardiac death.
- Extrinsic cardiomyopathies - cardiomyopathies where the primary pathology is outside the myocardium itself. Most cardiomyopathies are extrinsic, because by far the most common cause of a cardiomyopathy is ischemia. The World Health Organization calls these specific cardiomyopathies:
- Intrinsic cardiomyopathies - weakness in the muscle of the heart that is not due to an identifiable external cause.
- Dilated cardiomyopathy (DCM) - most common form, and one of the leading indications for heart transplantation. In DCM the heart (especially the left ventricle) is enlarged and the pumping function is diminished.
- Hypertrophic cardiomyopathy (HCM or HOCM) - genetic disorder caused by various mutations in genes encoding sarcomeric proteins. In HCM the heart muscle is thickened, which can obstruct blood flow and prevent the heart from functioning properly.
- Arrhythmogenic right ventricular cardiomyopathy (ARVC) - arises from an electrical disturbance of the heart in which heart muscle is replaced by fibrous scar tissue. The right ventricle is generally most affected.
- Restrictive cardiomyopathy (RCM) - least common cardiomyopathy. The walls of the ventricles are stiff, but may not be thickened, and resist the normal filling of the heart with blood. ** Noncompaction Cardiomyopathy - the left ventricle wall has failed to properly grow from birth and such has a spongy appearance when viewed during an echocardiogram.
Cardiovascular disease
- Cardiovascular disease is any of a number of specific diseases that affect the heart itself and/or the blood vessel system, especially the veins and arteries leading to and from the heart. Research on disease dimorphism suggests that women who suffer with cardiovascular disease usually suffer from forms that affect the blood vessels while men usually suffer from forms that affect the heart muscle itself. Known or associated causes of cardiovascular disease include diabetes mellitus, hypertension, hyperhomocysteinemia and hypercholesterolemia.
Types of cardiovascular disease include:
Congenital heart disease
- Congenital heart disease, existing primarily at birth, refers to any of a number of heart diseases caused by unavoidable genetic factors.
Coronary heart disease
- Coronary heart disease is a disease of the heart caused by the accumulation of atheromatous plaques within the walls of the arteries that supply the myocardium. Angina pectoris and myocardial infarction (heart attack) are symptoms of and conditions caused by coronary heart disease.
- Ischaemic heart disease - another disease of the heart itself, characterized by reduced blood supply to the organ.
Heart failure
- Heart failure, also called congestive heart failure (or CHF), and congestive cardiac failure (CCF), is a condition that can result from any structural or functional cardiac disorder that impairs the ability of the heart to fill with or pump a sufficient amount of blood throughout the body.
- Cor pulmonale, a failure of the right side of the heart.
Hypertensive heart disease
- Hypertensive heart disease, heart disease caused by high blood pressure, especially localised high blood pressure. Conditions that can be caused by hypertensive heart disease include:
- Left ventricular hypertrophy
- Coronary heart disease
- (Congestive) heart failure
- Hypertensive cardiomyopathy
- Cardiac arrhythmias
Inflammatory heart disease
Inflammatory heart disease involves inflammation of the heart muscle and/or the tissue surrounding it.
- Endocarditis - inflammation of the inner layer of the heart, the endocardium. The most common structures involved are the heart valves.
- Inflammatory cardiomyopathy
- Myocarditis - inflammation of the myocardium, the muscular part of the heart. It is generally due to infection (viral or bacterial). It may present with chest pain, rapid signs of heart failure, or sudden death.
Valvular heart disease
- Valvular heart disease is any disease process involving one or more valves of the heart. The valves in the right side of the heart are the tricuspid valve and the pulmonic valve. The valves in the left side of the heart are the mitral valve and the aortic valve.
Cholesterol Hazard
Cholesterol is a sterol (a combination steroid and alcohol). Cholesterol is a lipid found in the cell membranes of all tissues, and it is transported in the blood plasma of all animals. Because cholesterol is synthesized by all eukaryotes, trace amounts of cholesterol are also found in membranes of plants and fungi.
The name originates from the Greek chole- (bile) and stereos (solid), and the chemical suffix -ol for an alcohol, as researchers first identified cholesterol in solid form in gallstones by François Poulletier de la Salle in 1769. However, it is only in 1815 that chemist Eugène Chevreul named the compound "cholesterine".
Most of the cholesterol is synthesized by the body and some has dietary origin. Cholesterol is more abundant in tissues which either synthesize more or have more abundant densely-packed membranes, for example, the liver, spinal cord and brain. It plays a central role in many biochemical processes, such as the composition of cell membranes and the synthesis of steroid hormones. Cholesterol is insoluble in blood, but is transported in the circulatory system bound to one of the varieties of lipoprotein, spherical particles which have an exterior composed mainly of water-soluble proteins. The main types, low-density lipoprotein (LDL) and high-density lipoprotein (HDL) carry cholesterol from and to the liver.
According to the lipid hypothesis, abnormally high cholesterol levels (hypercholesterolemia) and abnormal proportions of LDL and HDL are associated with cardiovascular disease by promoting atheroma development in arteries (atherosclerosis). This disease process leads to myocardial infarction (heart attack), stroke and peripheral vascular disease. As high LDL contributes to this process, it is termed "bad cholesterol", while high levels of HDL ("good cholesterol") offer a degree of protection. The balance can be redressed with exercise, a healthy diet, and sometimes medication.
Cholesterol is excreted from the liver in bile and reabsorbed from the intestines. Under certain circumstances, when more concentrated, as in the gallbladder, it crystallises and is the major constituent of most gallstones, although lecithin and bilirubin gallstones also occur less frequently.
Abnormally low levels of cholesterol are termed hypocholesterolemia. Research into the causes of this state is relatively limited, and while some studies suggest a link with depression, cancer and cerebral hemorrhage it is unclear whether the low cholesterol levels are a cause for these conditions or an epiphenomenon.
Conditions with elevated concentrations of oxidized LDL particles, especially "small dense LDL" (sdLDL) particles, are associated with atheroma formation in the walls of arteries, a condition known as atherosclerosis, which is the principal cause of coronary heart disease and other forms of cardiovascular disease. In contrast, HDL particles (especially large HDL) have been identified as a mechanism by which cholesterol and inflammatory mediators can be removed from atheroma. Increased concentrations of HDL correlate with lower rates of atheroma progressions and even regression. The relation of cholesterol to CHD, termed the "lipid hypothesis," is still hotly debated.
Elevated levels of the lipoprotein fractions, LDL, IDL and VLDL are regarded as atherogenic (prone to cause atherosclerosis). Levels of these fractions, rather than the total cholesterol level, correlate with the extent and progress of atherosclerosis. Conversely, the total cholesterol can be within normal limits, yet be made up primarily of small LDL and small HDL particles, under which conditions atheroma growth rates would still be high. In contrast, however, if LDL particle number is low (mostly large particles) and a large percentage of the HDL particles are large, then atheroma growth rates are usually low, even negative, for any given total cholesterol concentration.
info : wikipedia
Saturday, November 10, 2007
headache
A headache (cephalgia in medical terminology) is a condition of pain in the head; sometimes neck or upper back pain may also be interpreted as a headache. It ranks amongst the most common local pain complaints.
The vast majority of headaches are benign and self-limiting. Common causes are tension, migraine, eye strain, dehydration, low blood sugar, and sinusitis. Much rarer are headaches due to life-threatening conditions such as meningitis, encephalitis, cerebral aneurysms, extremely high blood pressure, and brain tumors. When the headache occurs in conjunction with a head injury the cause is usually quite evident. A large percentage of headaches among females are caused by ever-fluctuating estrogen during menstrual years. This can occur prior to, during or even midcycle menstruation.
Treatment of uncomplicated headache is usually symptomatic with over-the-counter painkillers such as aspirin, paracetamol (acetaminophen), or ibuprofen, although some specific forms of headaches (e.g., migraines) may demand other, more suitable treatment. It may be possible to relate the occurrence of a headache to other particular triggers (such as stress or particular foods), which can then be avoided.
There are five types of headache: vascular, myogenic (muscle tension), cervicogenic, traction, and inflammatory.
Vascular
The most common type of vascular headache is migraine. Migraine headaches are usually characterized by severe pain on one or both sides of the head, an upset stomach, and, for some people, disturbed vision. It is more common in women. While vascular changes are evident during a migraine, the cause of the headache is neurologic, not vascular. After migraine, the most common type of vascular headache is the "toxic" headache produced by fever.
Other kinds of vascular headaches include cluster headaches, which cause repeated episodes of intense pain, and headaches resulting from high blood pressure (rare).
Muscular/myogenic
Muscular (or myogenic) headaches appear to involve the tightening or tensing of facial and neck muscles; they may radiate to the forehead. Tension headache is the most common form of myogenic headache.
Cervicogenic
Cervicogenic headaches originate from disorders of the neck, including the anatomical structures innervated by the cervical roots C1–C3. Cervical headache is often precipitated by neck movement and/or sustained awkward head positioning. It is often accompanied by restricted cervical range of motion, ipsilateral neck, shoulder, or arm pain of a rather vague non-radicular nature or, occasionally, arm pain of a radicular nature.
Traction/inflammatory
Traction and inflammatory headaches are symptoms of other disorders, ranging from stroke to sinus infection.
Specific types of headaches include:
- Tension headache
- Migraine
- Idiopathic intracranial hypertension (headache with visual symptoms due to raised intracranial pressure)
- Ictal headache
- "Brain freeze" (also known as: ice cream headache)
- Thunderclap headache
- Vascular headache
- Toxic headache
- Coital cephalalgia (also known as: sex headache)
- Hemicrania continua
- Rebound headache (also called medication overuse headache, abbreviated MOH)
- Red wine headache
- "Spinal headache" (or: post-dural puncture headaches) after lumbar puncture or related procedure that will lower the intracranial pressure
- Hangover (caused by heavy alcohol consumption)
A headache may also be a symptom of sinusitis.
Like other types of pain, headaches can serve as warning signals of more serious disorders. This is particularly true for headaches caused by inflammation, including those related to meningitis as well as those resulting from diseases of the sinuses, spine, neck, ears, and teeth.
info : wikipedia
















