Stroke (or cerebrovascular accident (CVA)) is the clinical designation for a rapidly developing loss of brain function due to an interruption in the blood supply to all or part of the brain. This phenomenon can be caused by thrombosis, embolism, or hemorrhage. In medicine, the process of being struck down by a stroke, fit, or faint is sometimes called an ictus [cerebri], from the Latin icere ("to strike"), especially prior to a definitive diagnosis.
Stroke is a medical emergency and can cause permanent neurological damage and death if not promptly diagnosed and treated. It is the third leading cause of death and the leading cause of adult disability in the United States and Europe. It is predicted that stroke will soon become the leading cause of death worldwide.
The symptoms of stroke can be quite heterogeneous, and patients with the same cause of stroke can have widely differing handicaps. Conversely, patients with the same clinical handicap can in fact have different underlying causes.
The cause of stroke causeing neurons to die or be seriously damaged, further impairing brain function.
Risk factors for stroke include advanced age, hypertension (high blood pressure), previous stroke or TIA (transient ischaemic attack), diabetes mellitus, high cholesterol, cigarette smoking, atrial fibrillation, migraine with aura, and thrombophilia. In clinical practice, blood pressure is the most important modifiable risk factor of stroke; however many other risk factors, such as cigarette smoking cessation and treatment of atrial fibrillation with anticoagulant drugs, are important.
Signs & Symptoms
The symptoms of stroke depend on the type of stroke and the area of the brain affected. Ischemic strokes usually only affect regional areas of the brain perfused by the blocked artery. Hemorrhagic strokes can affect local areas, but often can also cause more global symptoms due to bleeding and increased intracranial pressure.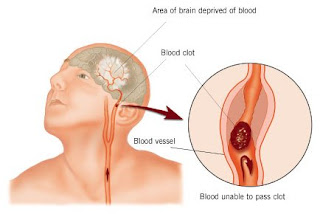
If the area of the brain affected contains one of the three prominent Central nervous system pathways—the spinothalamic tract, corticospinal tract, and dorsal column (medial lemniscus), symptoms may include:
- hemiplegia and muscle weakness of the face
- numbness
- reduction in sensory or vibratory sensation
In most cases, the symptoms affect only one side of the body. The defect in the brain is usually on the opposite side of the body (depending on which part of the brain is affected). However, the presence of any one of these symptoms does not necessarily suggest a stroke, since these pathways also travel in the spinal cord and any lesion there can also produce these symptoms.
In addition to the above CNS pathways, the brainstem also consists of the 12 cranial nerves. A stroke affecting the brainstem therefore can produce symptoms relating to deficits in these cranial nerves:
- altered smell, taste, hearing, or vision (total or partial)
- drooping of eyelid (ptosis) and weakness of ocular muscles
- decreased reflexes: gag, swallow, pupil reactivity to light
- decreased sensation and muscle weakness of the face
- balance problems and nystagmus
- altered breathing and heart rate
- weakness in sternocleidomastoid muscle with inability to turn head to one side
- weakness in tongue (inability to protrude and/or move from side to side)
If the cerebral cortex is involved, the CNS pathways can again be affected, but also can produce the following symptoms:
- aphasia (inability to speak or understand language from involvement of Broca's or Wernicke's area)
- apraxia (altered voluntary movements)
- visual field defect
- memory deficits (involvement of temporal lobe)
- hemineglect (involvement of parietal lobe)
- disorganized thinking, confusion, hypersexual gestures (with involvement of frontal lobe)
If the cerebellum is involved, the patient may have the following:
- trouble walking
- altered movement coordination
- vertigo and or disequilibrium
Loss of consciousness, headache, and vomiting usually occurs more often in hemorrhagic stroke than in thrombosis because of the increased intracranial pressure from the leaking blood compressing on the brain.
If symptoms are maximal at onset, the cause is more likely to be a subarachnoid hemorrhage or an embolic stroke.
Risk factors and prevention
Prevention of stroke can work at various levels including:
- primary prevention - the reduction of risk factors across the board, by public health measures such as reducing smoking and the other behaviours that increase risk;
- secondary prevention - actions taken to reduce the risk in those who already have disease or risk factors that may have been identified through screening; and
- tertiary prevention - actions taken to reduce the risk of complications (including further strokes) in people who have already had a stroke.
The most important modifiable risk factors for stroke are hypertension, heart disease, diabetes, and cigarette smoking. Other risks include heavy alcohol consumption (see Alcohol consumption and health), high blood cholesterol levels, illicit drug use, and genetic or congenital conditions. Family members may have a genetic tendency for stroke or share a lifestyle that contributes to stroke. Higher levels of Von Willebrand factor are more common amongst people who have had ischemic stroke for the first time. The results of this study found that the only significant genetic factor was the person's blood type. Having had a stroke in the past greatly increases one's risk of future strokes.
One of the most significant stroke risk factors is advanced age. 95% of strokes occur in people age 45 and older, and two-thirds of strokes occur in those over the age of 65. A person's risk of dying if he or she does have a stroke also increases with age. However, stroke can occur at any age, including in fetuses.
Sickle cell anemia, which can cause blood cells to clump up and block blood vessels, also increases stroke risk. Stroke is the second leading killer of people under 20 who suffer from sickle-cell anemia.
Men are 1.25 times more likely to suffer strokes than women, yet 60% of deaths from stroke occur in women. Since women live longer, they are older on average when they have their strokes and thus more often killed (NIMH 2002). Some risk factors for stroke apply only to women. Primary among these are pregnancy, childbirth, menopause and the treatment thereof (HRT). Stroke seems to run in some families.
Prevention is an important public health concern. Identification of patients with treatable risk factors for stroke is paramount. Treatment of risk factors in patients who have already had strokes (secondary prevention) is also very important as they are at high risk of subsequent events compared with those who have never had a stroke. Medication or drug therapy is the most common method of stroke prevention. Aspirin (usually at a low dose of 75 mg) is recommended for the primary and secondary prevention of stroke. Also see Antiplatelet drug treatment. Treating hypertension, diabetes mellitus, smoking cessation, control of hypercholesterolemia, physical exercise, and avoidance of illicit drugs and excessive alcohol consumption are all recommended ways of reducing the risk of stroke.
In patients who have strokes due to abnormalities of the heart, such as atrial fibrillation, anticoagulation with medications such as warfarin is often necessary for stroke prevention.
Procedures such as carotid endarterectomy or carotid angioplasty can be used to remove significant atherosclerotic narrowing (stenosis) of the carotid artery, which supplies blood to the brain. These procedures have been shown to prevent stroke in certain patients, especially where carotid stenosis leads to ischemic events such as transient ischemic attack. (The value and role of carotid artery ultrasound scanning in screening has yet to be established.)
info : wikipedia









No comments:
Post a Comment