Insulin Vs Diabetes
Insulin is an animal hormone whose presence informs the body's cells that the animal is well fed, causing liver and muscle cells to take in glucose and store it in the form of glycogen, and causing fat cells to take in blood lipids and turn them into triglycerides. In addition it has several other anabolic effects throughout the body.
Insulin is used medically to treat some forms of diabetes mellitus. Patients with type 1 diabetes mellitus depend on external insulin (most commonly injected subcutaneously) for their survival because of the absence of the hormone. Patients with type 2 diabetes mellitus have insulin resistance, relatively low insulin production, or both; some type 2 diabetics eventually require insulin when other medications become insufficient in controlling blood glucose levels.
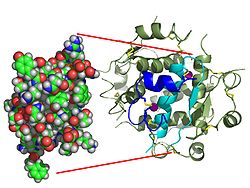
Insulin is a peptide hormone composed of 51 amino acid residues and has a molecular weight of 5808 Da. It is produced in the Islets of Langerhans in the pancreas. The name comes from the Latin insula for "island".
Insulin's genetic structure varies marginally between species of animal. Insulin from animal sources differs somewhat in regulatory function strength (i.e., in carbohydrate metabolism) in humans because of those variations. Porcine (pig) insulin is especially close to the human version.
In 1869 Paul Langerhans, a medical student in Berlin, was studying the structure of the pancreas (the jelly-like gland behind the stomach) under a microscope when he identified some previously un-noticed tissue clumps scattered throughout the bulk of the pancreas. The function of the "little heaps of cells," later known as the Islets of Langerhans, was unknown, but Edouard Laguesse later suggested that they might produce secretions that play a regulatory role in digestion. Paul Langerhans' son, Archibald, also helped to understand this regulatory role.
In 1889, the Polish-German physician Oscar Minkowski in collaboration with Joseph von Mering removed the pancreas from a healthy dog to test its assumed role in digestion. Several days after the dog's pancreas was removed, Minkowski's animal keeper noticed a swarm of flies feeding on the dog's urine. On testing the urine they found that there was sugar in the dog's urine, establishing for the first time a relationship between the pancreas and diabetes. In 1901, another major step was taken by Eugene Opie, when he clearly established the link between the Islets of Langerhans and diabetes: Diabetes mellitus … is caused by destruction of the islets of Langerhans and occurs only when these bodies are in part or wholly destroyed. Before his work, the link between the pancreas and diabetes was clear, but not the specific role of the islets.
Over the next two decades, several attempts were made to isolate whatever it was the islets produced as a potential treatment. In 1906 George Ludwig Zuelzer was partially successful treating dogs with pancreatic extract but was unable to continue his work. Between 1911 and 1912, E.L. Scott at the University of Chicago used aqueous pancreatic extracts and noted a slight diminution of glycosuria but was unable to convince his director of his work's value; it was shut down. Israel Kleiner demonstrated similar effects at Rockefeller University in 1919, but his work was interrupted by World War I and he did not return to it. Nicolae Paulescu, a professor of physiology at the University of Medicine and Pharmacy in Bucharest, published similar work in 1921 that had been carried out in France. Use of his techniques was patented in Romania, though no clinical use resulted.
In October 1920, Frederick Banting was reading one of Minkowski's papers and concluded that it is the very digestive secretions that Minkowski had originally studied that were breaking down the islet secretion(s), thereby making it impossible to extract successfully. He jotted a note to himself Ligate pancreatic ducts of the dog. Keep dogs alive till acini degenerate leaving islets. Try to isolate internal secretion of these and relieve glycosurea.
The idea was that the pancreas's internal secretion, which supposedly regulates sugar in the bloodstream, might hold the key to the treatment of diabetes.
He travelled to Toronto to meet with J.J.R. Macleod, who was not entirely impressed with his idea – so many before him had tried and failed. Nevertheless, he supplied Banting with a lab at the University, an assistant (medical student Charles Best), and 10 dogs, then left on vacation during the summer of 1921. Their method was tying a ligature (string) around the pancreatic duct, and, when examined several weeks later, the pancreatic digestive cells had died and been absorbed by the immune system, leaving thousands of islets. They then isolated an extract from these islets, producing what they called isletin (what we now know as insulin), and tested this extract on the dogs. Banting and Best were then able to keep a pancreatectomized dog alive all summer because the extract lowered the level of sugar in the blood.
Macleod saw the value of the research on his return but demanded a re-run to prove the method actually worked. Several weeks later it was clear the second run was also a success, and he helped publish their results privately in Toronto that November. However, they needed six weeks to extract the isletin, which forced considerable delays. Banting suggested that they try to use fetal calf pancreas, which had not yet developed digestive glands; he was relieved to find that this method worked well. With the supply problem solved, the next major effort was to purify the extract. In December 1921, Macleod invited the biochemist James Collip to help with this task, and, within a month, the team felt ready for a clinical test.
On January 11, 1922, Leonard Thompson, a 14-year-old diabetic who lay dying at the Toronto General Hospital, was given the first injection of insulin. However, the extract was so impure that Thompson suffered a severe allergic reaction, and further injections were canceled. Over the next 12 days, Collip worked day and night to improve the ox-pancreas extract, and a second dose injected on the 23rd. This was completely successful, not only in not having obvious side-effects, but in completely eliminating the glycosuria sign of diabetes.
Children dying from diabetic keto-acidosis were kept in large wards, often with 50 or more patients in a ward, mostly comatose. Grieving family members were often in attendance, awaiting the (until then, inevitable) death. In one of medicine's more dramatic moments Banting, Best and Collip went from bed to bed, injecting an entire ward with the new purified extract. Before they had reached the last dying child, the first few were awakening from their coma, to the joyous exclamations of their families.
However, Banting and Best never worked well with Collip, regarding him as something of an interloper, and Collip left the project soon after.
Over the spring of 1922, Best managed to improve his techniques to the point where large quantities of insulin could be extracted on demand, but the preparation remained impure. The drug firm Eli Lilly and Company had offered assistance not long after the first publications in 1921, and they took Lilly up on the offer in April. In November, Lilly made a major breakthrough, and were able to produce large quantities of purer insulin. Insulin was offered for sale shortly thereafter.
Oral insulin
The basic appeal of oral hypoglycemic agents is that most people would prefer a pill to an injection. However, insulin is a protein. Proteins, eg meat proteins, are digested in the stomach and gut and insulin, being a protein, is no exception.
The potential market for an oral form of insulin is assumed to be enormous, thus many laboratories have attempted to devise ways of moving enough intact insulin from the gut to the portal vein to have a measurable effect on blood sugar. One can find several research reports over the years describing promising approaches or limited success in animals, and limited human testing, but as of 2004, no products appear to be successful enough to bring to market.[9]
Pancreatic transplantation
Another improvement would be a transplantation of the pancreas or beta cell to avoid periodic insulin administration. This would result in a self-regulating insulin source. Transplantation of an entire pancreas (as an individual organ) is difficult and relatively uncommon. It is often performed in conjunction with liver or kidney transplant, although it can be done by itself. It is also possible to do a transplantation of only the pancreatic beta cells. It has been highly experimental (for which read 'prone to failure') for many years, but some researchers in Alberta, Canada, have developed techniques with a high initial success rate (about 90% in one group). Nearly half of those who got an islet cell transplant are insulin-free one year after the operation; by the end of the second year that number drops to about one in seven. Beta cell transplant may become practical in the near future. Additionally, some researchers have explored the possibility of transplanting genetically engineered non-beta cells to secrete insulin. Clinically testable results are far from realization at this time. Several other non-transplant methods of automatic insulin delivery are being developed in research labs, but none is close to clinical approval.
info : wikipedia









No comments:
Post a Comment